Written by Jacquie Moore, BA’97
Three or four years ago, an interesting thing happened to gut health. From the science behind it to the foods required to keep it thriving, the community of micro-organisms that live inside our bodies reached cocktail party-conversation status. Indeed, it’s virtually impossible to turn on the TV or walk through a grocery store without seeing the promotion of probiotics, skincare products, drink powders, packaged snacks and cookbooks claiming improved gut health (legit or not).
It was about time “microbiome” became a household word: more than 2,000 years ago, Hippocrates, the father of modern medicine, proclaimed that “all diseases begin in the gut.” A growing body of research proves he wasn’t far off.
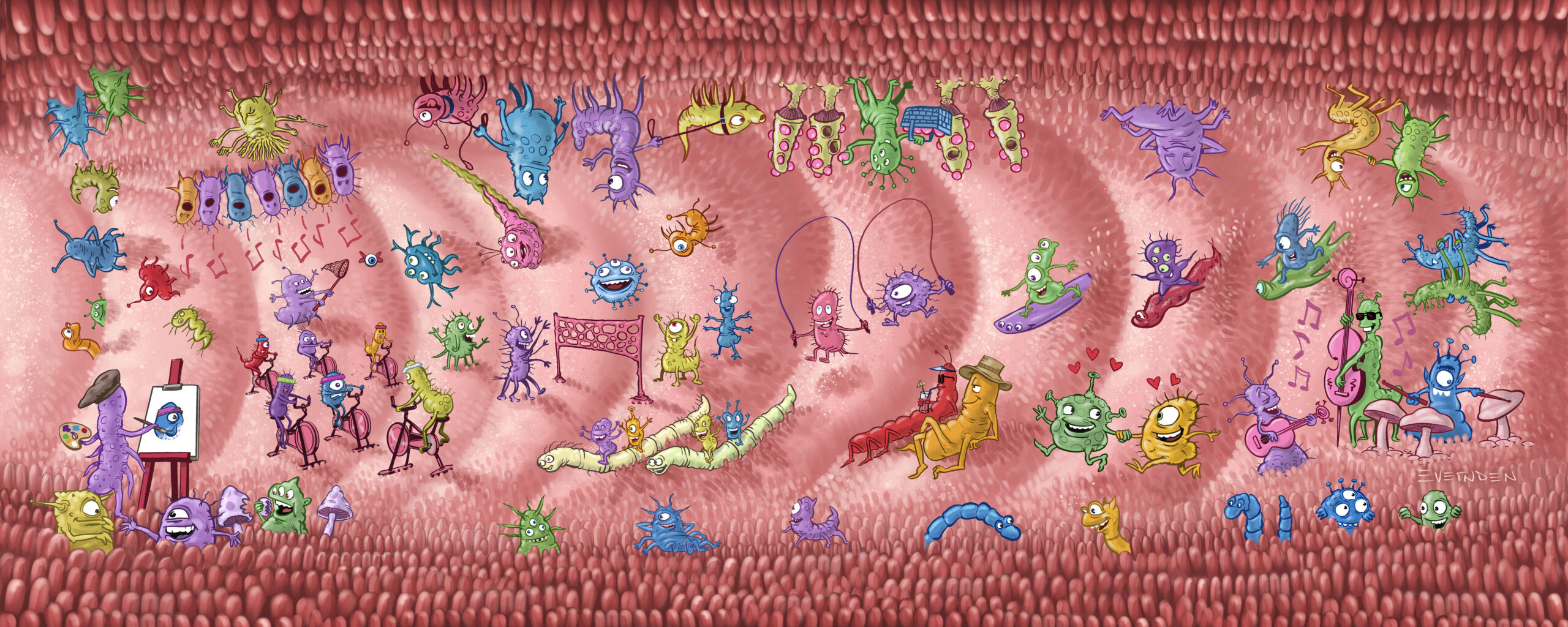
The “gut” is shorthand for the entire, highly complex digestive tract. The word microbiome refers to the collection of trillions of microbes and their activities — sometimes called their “theatre of activity,” referring to microbial structures, metabolites, genes, etc. — is found mostly in our gut and in and around other areas of our bodies. These bacteria, parasites, viruses and fungi play a major role in shaping and educating our immune systems. Every person has a unique microbiome that plays an instrumental role in health and wellness, protecting us from pathogens and chronic diseases such as cancer, cardiovascular disease, diabetes, asthma, inflammatory bowel disease and chronic infections.
Not surprisingly, the quest to unlock the mysteries of the gut microbiome is considered one of the most important scientific pursuits in human health this century. University of Calgary experts at the global forefront of transformative microbiome discovery are asking, and answering, profound questions to change the future of health.
The Centre to Study it All
Dr. Kathy McCoy, PhD, is a professor of physiology and pharmacology in the Cumming School of Medicine (CSM), as well as the scientific director of UCalgary’s renowned International Microbiome Centre (IMC). The IMC is a hub for translational gut-health research, designed to investigate the microbiome of humans, plants, animals and the physical environment. Its germ-free facility, biobank and real-time imaging lab, as well as its partnership with the Snyder Institute for Chronic Diseases, Hotchkiss Brain Institute (HBI), Alberta Children’s Hospital Research Institute, and other labs and departments, support cutting-edge discovery. McCoy and her team, as well as colleagues from a variety of disciplines across UCalgary, are empowered to work toward their ultimate purpose to, as McCoy says, “harness the microbiome to better treat and prevent disease.” Already, their work has shed light on the profound role of the gut microbiome in our physical and mental health.
The Gut and Mental Health
The gut-brain connection isn’t “just a feeling;” it’s an evidence-based, two-way connection. Indeed, the brain is shaped by bacteria in the digestive tract. A stressed intestine can send signals to the brain, and a stressed brain can send signals to the gut. It’s no surprise, then, that a troubled intestine can be the cause or the product of anxiety and/or depression. While fecal transplant capsules are already used to treat dangerous gut infections (such as Clostridium difficile), they are not yet approved to treat mental illness — though that may happen in the future.

Dr. Valerie Taylor, MD, PhD, a professor of psychiatry in the CSM, is one of the few funded researchers in the world examining the therapeutic effects of fecal transplant as a treatment for depression and other mental illness.
“Our work is asking, ‘Can we alter the gut microbiome and improve mental illness symptoms?’” says Taylor, who runs the largest biological neuroscience microbiome repository in North America. “We have already explored bipolar disorder, and now we’re looking at depression and irritable bowel syndrome.”
Her lab also has plans to examine obsessive-compulsive disorder and the microbiome. In partnership with the HBI and the Snyder Institute, Taylor and her team are overseeing blended clinical trials in their aim to design treatment for mental health by changing the gut microbiota.
“We have more serotonin receptors in our gastrointestinal system than in our brain,” says Taylor. “We have assumed that depression and other mental disorders are brain illnesses because that’s where we think emotion is regulated, but it may be much more complicated than that.”
Diet and Gut Inflammation
More than 250,000 people in Canada are currently living with Crohn’s or ulcerative colitis, collectively referred to as inflammatory bowel diseases (IBD). Up to 50 per cent of patients with IBD may not respond to usual treatments or eventually lose response to their therapies. There’s desperate need for new treatment options to improve the debilitating symptoms and complications of these diseases.
Gastroenterologist and associate professor Dr. Maitreyi Raman, MSc’08, MD, is exploring the evolving area of research around dietary interventions. While some research has explored the link between food and quality of life for patients with Crohn’s disease, diet guidelines for IBD treatment have been lacking — until recently. Raman says she is “immensely interested in the role of diet and how it can modify inflammation, and how diet may impact the gut microbiome.”
Existing data confirms that certain foods are, indeed, associated with inflammation in the intestines in some individuals, but Raman and her team are pushing the question further by testing different diets and examining other factors that may lead to changes in the microbiome, and whether microbiome changes may improve the course of gut inflammation.
“If we can alter the ‘bad’ microbes (pathogens) or ‘decolonize’ them and replace them with beneficial ones, we think we can modify how the gut responds to inflammation,” Raman says. Her team recently published food pyramid guidelines recommending certain priority behaviours for people diagnosed with IBD; eating certain foods (leafy greens and multicoloured fruit and veg) and avoiding others (sugar) can potentially extend remission time.
To help people make such healthy changes to their diet with a little more ease, Raman and her team recently translated their evidence-based data into a digital mobile app. Named LyfeMD, the app helps patients through a system of information, tools and personalized health coaching; it’s tough to argue with its tagline: “You deserve to be the happiest, healthiest you.”
The Gut Connection Between Babies and Their Dad
For the past several years, scientists have explored ways to improve infant health by improving the microbiome of the expectant mother. In UCalgary’s Faculty of Kinesiology, Dr. Raylene Reimer, PhD, has done extensive research to study how diet during pregnancy, particularly prebiotics, influences offspring’s gut microbiota, glucose tolerance and, ultimately, obesity risk. Given that most babies get their first significant dose of microbes when they pass through the birth canal, it’s a critical area of exploration that, says Reimer, “researchers keep coming back to as we discover more about it.” Recently, however, she’s been compelled by a new angle: how does the father’s microbiome come into play?
In a recent talk to the Canadian Nutrition Society, Reimer presented data from a Swedish epidemiological study that linked longevity and disease to nutrition in paternal ancestors. “There was excellent record-keeping in a northern region in Sweden in the 1800s in terms of harvest and grain yields, and the food supply that was available from year to year,” she said. It seems that the grandchildren of boys who had access to an excess food supply when they were between the ages of nine and 12 (i.e., over-nutrition during the slow-growth phase of their adolescence) had a significantly increased chance of diabetes-related death. On the other hand, grandkids of boys in that age group who had poor food availability inadvertently protected their future offspring from cardiovascular disease.
Reimer and her team of graduate students are currently studying rats to learn more about the link between a father’s nutrition around the time of conception, and how the microbiota of seminal fluid is modifiable by diet.
Exercise and Gut Health
Because we can always use at least one more reason to get out the bike/runners/racquet/leotard or whatever your workout-jam might be, a new study led by a PhD candidate in the Faculty of Kinesiology demonstrates that exercise is good for the gut (and, no, we don’t just mean in the quest for a six-pack). Student Kate Sales’ bi-directional research looks at both the impact of different types and intensities of exercise on the structure of the gut microbiota, as well as at the influence of a probiotic intervention on endurance exercise performance.

She and her team recently completed a six-week training project, for which participants engaged in a variety of low-to-high-intensity cycling exercise three times a week. “We looked for changes in the abundance of different bacteria in the gut, and a change in the concentration of certain metabolites produced by the ‘good’ bacteria in the gut,” says Sales, BKin’16, MKin’19.
Her next, double-blind study will gather data from trained cyclists — half of them taking a probiotic to see if supplementation triggers changes in metabolism, VO2max, peak power output, etc. Sales’ data contributes to a growing body of research that illuminates the significance of a personalized approach to the microbiome.
“The big questions are, ‘What is a good microbiome?’ and, ‘What is a bad microbiome?” Sales says. “While that’s different from person to person, I want to learn how different types of exercise can influence our gut microbiota — and how this information could be leveraged when developing exercise programs for disease-improvement and prevention.”
Preventing Future Health Issues in Premature Babies
About 11 per cent of babies worldwide are born prematurely, before 37 weeks gestation — and most of those arrive between 32 and 36 weeks. While babies can safely be born even earlier, between 26 and 32 weeks, they may need special care to support their development.
“Their systems are immature and these babies are at risk of developing health conditions such as asthma, allergies and obesity,” says Dr. Marie-Claire Arrieta, PhD, an associate professor in the departments of Physiology & Pharmacology and Paediatrics. Arrieta, who has been involved in microbiome research for more than a decade, is interested in unlocking the ways in which an immature microbiome may contribute to health concerns such as asthma. “We’re just at the beginning of learning how the microbiome contributes to a baby’s health or disease, and how we can restore a premature baby’s microbiome in a safe way.”
Currently, the analysis of a baby’s microbiome can take several weeks, as it calls for extensive genomic sequencing. Arrieta and her team are working to develop rapid, bedside methods so that a doctor can quickly detect a “bad” microbiome and immediately make an informed decision for how to feed and treat a preemie. It could be a tiny, but mighty intervention that may save lives.
The Fungus Among Us
While bacteria have always received the most attention from gut-microbiome researchers, fungus has lately found a brighter place under the microscope. “The role of fungi is little-known so far, but we know they interact with our immune system, and they are just as important as any other member of the microbiome in shaping that ecosystem,” says Arrieta.
Although Arrieta was mainly studying the microbiome signatures in babies, a few years ago, she was moved enough by a conference presentation studying fungi to ask herself, “Why I wasn’t doing the same thing with fungi as I do with bacteria?”
Separating fungi from their gut community is an enormously time-consuming and challenging task that is, says Arrieta, possible in very few labs around the world; the experimental suites in the IMC’s germ-free facility enable her and her team to tease apart and analyze the direct effects of fungi from those driven by bacteria. So far, her research shows that fungi work alongside bacteria to send important signals from the gut to the brain and holds great potential for prevention and treatment of many chronic diseases.
EXTRA CREDIT
Dr. Braedon McDonald, PhD’13, MD’13, and his colleagues found that the high rates of infection in critically ill patients are linked with abnormalities of the microbiome in conjunction with an impaired immune system. Read more in UCalgary News.
Research by Dr. Kathy McCoy, PhD, discovered which gut bacteria help our immune system battle cancerous tumours and how they do it. Read more at UCalgary News.
See inside the International Microbiome Centre. Watch the video.