Written by Jacquie Moore, BA’97
Illustrated by Vidhya Nagarajan
In 1911, one “Mrs. Chase” arrived at a Connecticut hospital. Perpetually rosy-cheeked and dressed in a demure cotton nightgown, she was Patient Zero in an experiment designed to improve health-care practice.
Before she came along, nurses had been getting hands-on experience on the fly, attending to real injured people in clinics and on battlefields. Mrs. Chase came to the hospital with stitches in her knees, elbows, shoulders and hips — she was a life-sized manikin, the first “doll” designed for training nurses. She, and her modern-day descendants in simulated hospital settings around the world, transformed nursing education.
The University of Calgary’s Clinical Simulation Learning Centre (CSLC, or “the sim centre”) in the Faculty of Nursing is delivering increasingly true-to-life experiences to students poised to embark on health-care careers with deeper knowledge and more finely honed practical skills than ever before. For third-year nursing student Fabricio Abril, the sim centre’s diverse family of uncannily lifelike manikin-patients have significantly advanced his learning (and, not incidentally, shifted his perspective on babies thanks to what might be Mrs. Chase’s great-great-great-grandbaby).
In his first year of nursing, Abril, along with his cohort, visited real people in a local nursing home, which he found gratifying and illuminating. He was therefore skeptical when, in second year, they were introduced to the idea of training in the sim centre. “I was, like, ‘Manikins? What? How can I learn with a manikin?’” He changed his tune when faced with the Lucina Childbirth Simulator (her friends call her Lucina), a high-fidelity, wireless manikin with integrated maternal-fetal physiology that breathes, bleeds and mechanically gives birth to a 2.5-kg sim baby.
On one occasion, following instruction and preparation in the sim centre, Abril and a small group were left to take care of postpartum Lucina while their instructors took their places behind the one-way glass that separates the simulated hospital room from a control booth. “We were so nervous — it’s incredible that it’s a manikin because it all feels so real, we were sweating and shaking,” he says. The students checked vitals (controlled by the trained behind-the-scenes simulation instructors) and talked to the patient (who talks back via the same instructors).
When Lucina began to hemorrhage, Abril panicked.
“There’s protocol in hospitals when a nurse calls for help — state your name, the patient’s name, the room, etc. — but, instead of using calm language and codes, which I didn’t yet know, I just picked up the phone and yelled, ‘She’s bleeding!’” Abril laughs at himself as he recalls the incident, but he’s grateful for the opportunity to have viscerally felt the importance of hands-on, in-the-moment training.
Given that Abril and his classmates sometimes feel genuine life-or-death anxiety in the sim-suite, it’s fortunate that they are not additionally burdened by the stress of high-stakes testing. The centre’s philosophy emphasizes learning rather than performance, which is often attached to grades, says Carla Ferreira, BN’03, senior instructor and the nursing practice simulation co-ordinator. “The experiences here are based on formative assessment that allows students to build practical skills as well as assertiveness in speaking up about what might not be working,” she says.
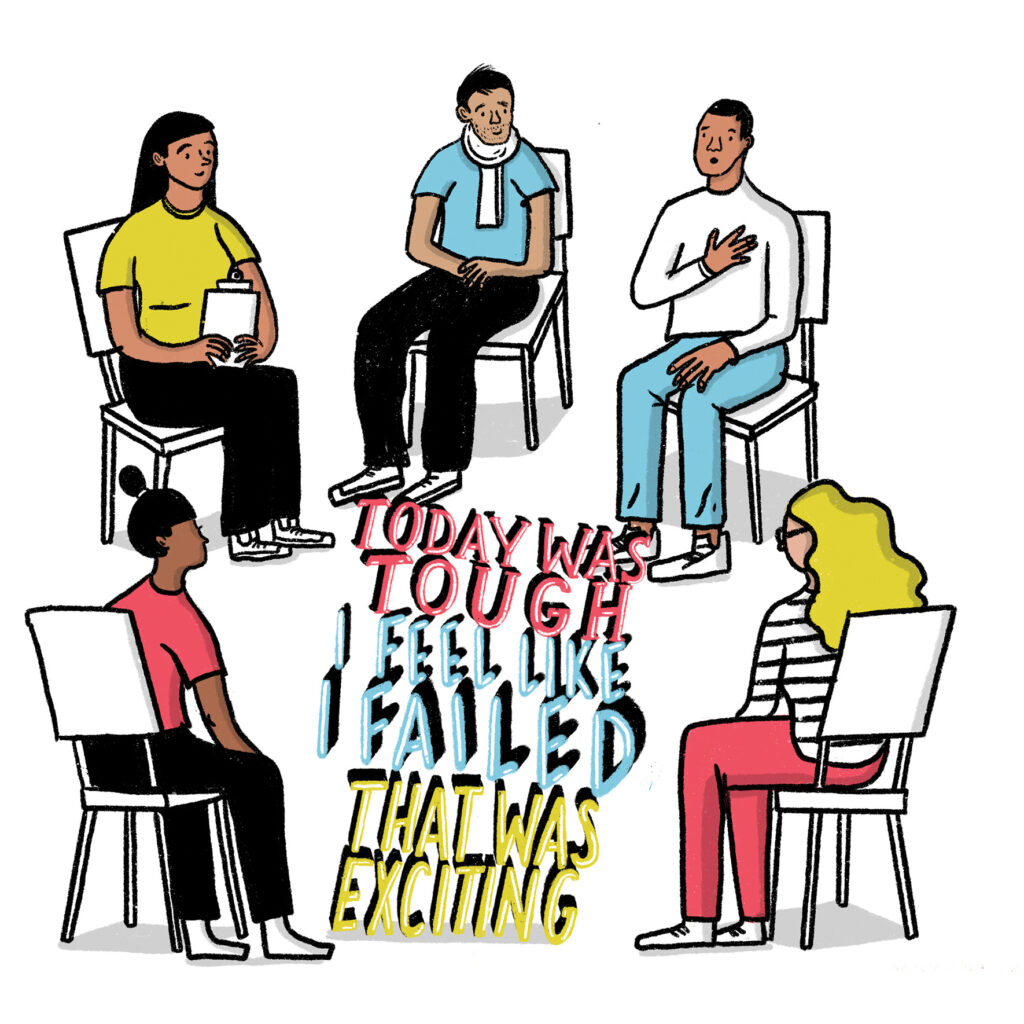
After each simulation-based learning, the participating group of students and the simulation instructor settle into a debriefing room to discuss not only what went right, and what didn’t, but more importantly why. For Abril, that process was another transformative moment.
“I thought, ‘Oh, I shouldn’t highlight the mistakes I made to draw more attention to where I failed,’” he says. “But right away I realized that, no, it’s the opposite: nurses benefit from learning to be vulnerable and fearless by sharing and talking about how we felt in a situation and what we experienced so that we can do better. We need to learn to process and let go of things so that we don’t carry that with us to the next patient.”
Ultimately, a successful learning experience in a nursing simulation centre pivots on a student’s ability to suspend their disbelief. Sure, the medical instruments are fake; the numbers on the vital sign monitors are controlled by instructors; Rubbermaid bins hold spare limbs and abdominal wounds; and, of course, the patients are made in a factory. But, evidence shows, the more a student can buy in to a scenario, the more likely it is that they’ll achieve learning goals, increase their confidence and skills, and retain what they learn. The centre occasionally hires actors to play patients, which is one way of circumventing the challenge of creating realistic sims, but, as the sim centre’s manager, Jeff Dawes, points out, “You can’t stick an IV in an actor’s arm or give them a broken leg.”
Unfortunately, stiff-limbed Mrs. Chase, along with the majority of contemporary manikins that tend to be modelled on younger, light-skinned, anatomically ideal individuals don’t cut it anymore, says Ferreira. While mechanically speaking they are certainly useful training tools — most come with built-in electronic components that allow for lifelike functions including blinking and breathing — they don’t quite hit the emotional buttons. “We need to realistically reflect Calgary’s community, the people nurses will be caring for,” she says. With that crucial goal in mind, sim centre faculty and staff do their best to diversify the look of existing manikins using makeup and wigs, but they can only do so much. “If we’re asking students to imagine they’re talking to an 80-year-old individual, it’s distracting for them to have to ‘remember’ that when what they’re looking at resembles a younger person,” says Ferreira.
Thankfully, the medical-simulation industry is making progress on this front. Last year, Dawes was able to order two EchoMasks — highly realistic, medical-grade silicone masks that fit over existing manikin heads. The skin tone of the masks is darker, and the faces look more aged than the smooth white manikin faces beneath. Dawes recently ordered two more masks meant to resemble the faces of senior Asian individuals.
Ferreira says she’s cognizant of the fact that, no matter how true-to-life the manikins are, “we are only representing what we can see on the outside.” That’s true, of course, but, as Abril experienced, sometimes what we see on the outside can have a startlingly moving effect on how we feel on the inside.
When Abril — who admits he had never been particularly interested in babies — first held an uncannily realistic Lifecast infant, he was surprised and delighted (the centre’s family of Lifecast-brand manikins are the most eerily lifelike on the market, but they don’t have the electronic components of their high-fidelity brethren).
“Most of the girls in the group had experience holding babies, but the guys didn’t,” he says. “My sister likes babies, I didn’t really. But when I picked up that baby? She’s amazing.” Smitten, Abril named her Theresa. “She made me like babies.”
Inside the Sim Centre
Students get to learn and fail and learn some more under the direction of instructors who set real-life scenarios, from taking care of a sim mother and baby to understanding how to communicate with a medical team in a hospital setting